New Developments in Sickle Cell Anemia Care
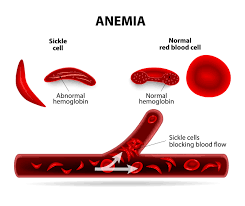
Sickle cell anaemia is a genetic blood disorder characterised by the abnormal production of haemoglobin, a protein responsible for carrying oxygen in red blood cells. This condition is inherited when a person receives two copies of the abnormal haemoglobin gene, one from each parent. Normally, red blood cells are flexible and round, allowing them to easily move through blood vessels. However, in individuals with sickle cell anaemia, the abnormal haemoglobin causes red blood cells to become rigid, sticky, and take on a crescent or sickle shape. These abnormal cells can easily get trapped and block blood flow in small blood vessels, leading to various complications.
 |
| Sickle cell disease |
Some of the common symptoms and complications of sickle cell anaemia include:
- Pain crises: Episodes of severe pain due to blocked blood flow, especially in the bones, joints, chest, and abdomen.
- Anaemia: Sickle cells have a shorter lifespan than normal red blood cells, leading to a shortage of healthy red blood cells and anaemia, which can cause fatigue, weakness, and shortness of breath.
- Increased risk of infections: Sickle cell anaemia can weaken the immune system, making individuals more susceptible to infections, particularly bacterial infections.
- Organ damage: Repeated episodes of blocked blood flow can cause damage to organs such as the lungs, kidneys, liver, and spleen.
- Stroke: Sickle cells can block blood vessels in the brain, leading to a stroke.
- Eye problems: Sickle cell anaemia can affect the blood vessels in the eyes, potentially causing vision problems or even blindness.
- Delayed growth and development: Chronic anaemia and complications of sickle cell disease can interfere with normal growth and development, particularly in children.
What are the types of Sickle cell disease?
There are several types of sickle cell illness, also known as sickle cell disease (SCD), which are variations of the condition based on the specific genetic inheritance. The main types of sickle cell illness include:
- Sickle Cell Anaemia (HbSS): This is the most common and severe form of SCD. Individuals with sickle cell anaemia inherit two abnormal haemoglobin S (HbS) genes, one from each parent. This results in the production of primarily sickle haemoglobin (HbS) in red blood cells.
- Sickle-Haemoglobin C Disease (HbSC): In this type, individuals inherit one HbS gene and one abnormal haemoglobin C (HbC) gene. HbSC disease is generally milder than sickle cell anaemia but still presents symptoms and complications.
- Sickle Beta-Plus Thalassemia (HbS/β+ Thalassemia): This form occurs when an individual inherits one HbS gene and one gene for beta-thalassemia. Thalassemias are a group of inherited blood disorders that affect the production of haemoglobin. Sickle beta-plus thalassemia can have variable severity, with symptoms ranging from mild to moderate.
- Sickle Beta-Zero Thalassemia (HbS/β0 Thalassemia): In this type, individuals inherit one HbS gene and one gene for beta-thalassemia with absent or severely reduced beta-globin production. Sickle beta-zero thalassemia typically has more severe symptoms and complications compared to other forms of SCD.
How is sickle cell anaemia treated?
The treatment of sickle cell anaemia aims to manage symptoms, prevent complications, and improve the quality of life for individuals with the condition. The treatment approach may vary depending on the specific symptoms and severity of the disease. Here are some common strategies and interventions used in the management of sickle cell anaemia:
The treatment of sickle cell anaemia aims to manage symptoms, prevent complications, and improve the quality of life for individuals with the condition. The treatment approach may vary depending on the specific symptoms and severity of the disease. Here are some common strategies and interventions used in the management of sickle cell anaemia:
- Pain management: Pain crises are a hallmark of sickle cell anaemia. Pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, are often used to manage acute pain episodes. Intravenous fluids and heat application can also help alleviate pain.
- Hydroxyurea: This medication is commonly prescribed for individuals with sickle cell anaemia. It helps increase the production of fetal haemoglobin, which can prevent the sickling of red blood cells and reduce the frequency of pain crises. Hydroxyurea requires close monitoring and regular blood tests.
- Blood transfusions: Regular blood transfusions can help increase the number of healthy red blood cells and reduce the risk of complications. Transfusions are typically used for severe cases or to manage specific complications, such as stroke or acute chest syndrome.
- Antibiotics and vaccinations: People with sickle cell anaemia have an increased risk of infections. Antibiotics may be prescribed to prevent or treat bacterial infections. Vaccinations, including pneumococcal, meningococcal, and influenza vaccines, are also recommended to reduce the risk of infections.
- Folic acid supplementation: Folic acid helps in the production of new red blood cells. Supplementation with folic acid is often prescribed to individuals with sickle cell anaemia to support red blood cell production.
- Bone marrow or stem cell transplantation: In severe cases of sickle cell anaemia, bone marrow or stem cell transplantation may be considered. This procedure involves replacing the bone marrow with healthy donor cells, which can produce normal red blood cells. Transplantation carries risks and is typically reserved for individuals with severe symptoms or complications.
- Pain management techniques: Non-medication approaches, such as relaxation techniques, heat therapy, and distraction techniques, may also be used to help manage pain during crises.
What are the recent updates in sickle cell anaemia treatment?
However, it's important to note that medical research is constantly evolving, and there may have been further developments since then. Here are some notable updates:
However, it's important to note that medical research is constantly evolving, and there may have been further developments since then. Here are some notable updates:
- Gene Therapy: Gene therapy has shown promising results in the treatment of sickle cell anaemia. The technique involves modifying a patient's own stem cells to produce normal haemoglobin and prevent the sickling of red blood cells. Clinical trials have demonstrated significant reductions in the frequency of vaso-occlusive crises and transfusion requirements in some patients.
- Crispr-Cas9: The gene-editing tool Crispr-Cas9 holds potential for treating sickle cell anaemia. Researchers have been exploring its application to correct the genetic mutation responsible for sickle cell disease, potentially offering a cure. Although still in the early stages, preclinical studies and initial clinical trials have shown promising results.
- Targeted Therapies: New targeted therapies are being developed to specifically address the underlying mechanisms of sickle cell anaemia. These therapies aim to inhibit or modulate certain molecules and pathways involved in the sickling process, reducing the frequency and severity of symptoms. Examples include drugs targeting selectins, adhesion molecules, and inflammation pathways.
- Improved Pain Management: Efforts have been made to enhance pain management strategies for sickle cell patients. This includes the development of novel pain medications, the optimisation of existing analgesics, and the exploration of non-pharmacological approaches such as virtual reality therapy and psychological interventions.
Tags
Sickle Cell Anemia